Teamwork and Telehealth: Seattle Shows the Way in Early Pandemic Response
Physical distancing is our first and primary weapon against COVID-19. Wielding it early and with unwavering commitment is flattening the curve in places where the virus emerged first in the U.S. The early experience from Seattle, and the generosity of its public and private institutions to share their learnings and collaborate in real time, is guiding decisions and strategies across the country. Their efforts highlight how — in addition to local public actions like physical distancing — it is also important to have a healthcare delivery system that has a strong foundation in telehealth, digital communication and care coordination.
Community Assets, Collaboration Support Resilience
In many ways, the rest of us are fortunate that COVID-19 emerged first in Seattle. The presence of deep expertise in medicine, research, health care delivery, technology, and public sector leadership, and a tradition of collaboration has come together in Washington State to produce and disseminate valuable knowledge. The area’s history of team-based, tech-enabled integrated care delivery and multispecialty medical groups has also served it well at this critical moment.
Providence Regional Medical Center in Everett diagnosed the first case of COVID-19 in January, but community spread was already happening. Researchers studying Seattle seasonal flu patterns recognized quickly that their surveillance system could help identify the path of the virus, but faced regulatory hurdles in turning their diagnostic skills on the novel coronavirus. Epidemiologists at the Institute for Health Metrics and Evaluation at the University of Washington, launched and supported by the Bill and Melinda Gates Foundation, developed a model that is now being used by many other health systems and public health leaders to forecast the path of the virus in their own communities and plan for the surge in cases.
The University of Washington has served as the primary testing lab, and Washington has steadily ramped up its testing capacity. The Kaiser Permanente Washington Research Institute has already become a site for a clinical trial of a COVID-19 vaccine and given injections to the first volunteers.
At the Everett Clinic, a Council of Accountable Physician Practices (CAPP) medical group, Dr. Yuan-P Tu rallied parent company Optum to expedite testing of a simpler self-administered swab test for detecting COVID-19 which has been FDA approved. This was an extraordinary partnership between the Bill & Melinda Gates Foundation, the University of Washington, Quest Diagnostics, and UnitedHealth Group Research and Development. Under the new testing method, the swab can be patient-administered at the front of the nose and handed back to the health care worker. “This is groundbreaking, because it will radically change how the samples are obtained and make the health care worker much safer,” Dr. Tu said.
Rapid and Sustained Leadership Response
The deadly path that the virus took through a nursing home in February in Kirkland, Washington, helped to galvanize attention and response not just in Seattle, but in other metropolitan areas. Social distancing measures began in early March in the city when the mayor declared a state of emergency, and later extended across the state. While the outbreak has been deadly and has stressed the care delivery system, the rate of transmission is slowing, which allows for more surge capacity, the ability to obtain more equipment and supplies, and most importantly, and the ability to better protect health care workers.
Kaiser Permanente Washington and the Washington Permanente Medical Group (another CAPP group) already a leader in providing telehealth, scaled up the amount of care delivered virtually to over 50%, keeping as many patients as possible safely in their homes. Virtual care options include e-visits, consulting nurse services, care chat online messaging, and video and phone visits. While urgent care facilities remain open to triage symptomatic patients, many facilities have been temporarily closed to minimize the risk of infection and preserve protective equipment for health care workers. Kaiser Permanente allowed early prescription refills and mail delivery of medications to minimize avoidable trips to the pharmacy, and as of this writing has seven COVID-19 testing sites in the region.
By offering a broader array of virtual capabilities, we’re showing our patients that we’re here for them to provide the right care at the right time, especially in a moment of uncertainty and crisis. Our moment is now to truly slow the spread of this deadly virus,” said Paul Minardi, MD, president and executive medical director of Washington Permanente Medical Group.
Planning and Positioning Surge Capacity
Kaiser Permanente and its partner hospitals at Swedish have participated in the Northwest Healthcare Response Network, a nonprofit coalition “driving disaster preparedness and response.” This network of providers, first responders, public health departments, and Tribal Nations have been planning, training, and simulating disaster response since 2005. The coalition can track bed capacity and support collaboration across institutions.
Here is how King County Department of Public Health described the situation at the end of March:
“The unprecedented steps our hospitals have taken are helping ensure hospital and ICU bed and ventilator capacity remain available in the region at this time. Hospitals have responded to the increase in patients with COVID-19 and COVID-like illnesses by using surge strategies, such as postponing elective and non-emergency procedures, bringing in additional staff, and increasing the number of hospital beds. Other innovative changes to managing healthcare needs while decreasing opportunities for transmission of COVID-19 include drive through clinics and telehealth.”
Microsoft lent its technical support to Swedish Health Services by building an app that helps hospital staff monitor resources for COVID-19 related care. Frontline workers can use mobile devices to keep track of patients, protective gear, ventilator use, and other COVID-related information, and it’s already helping identify capacity for more care.
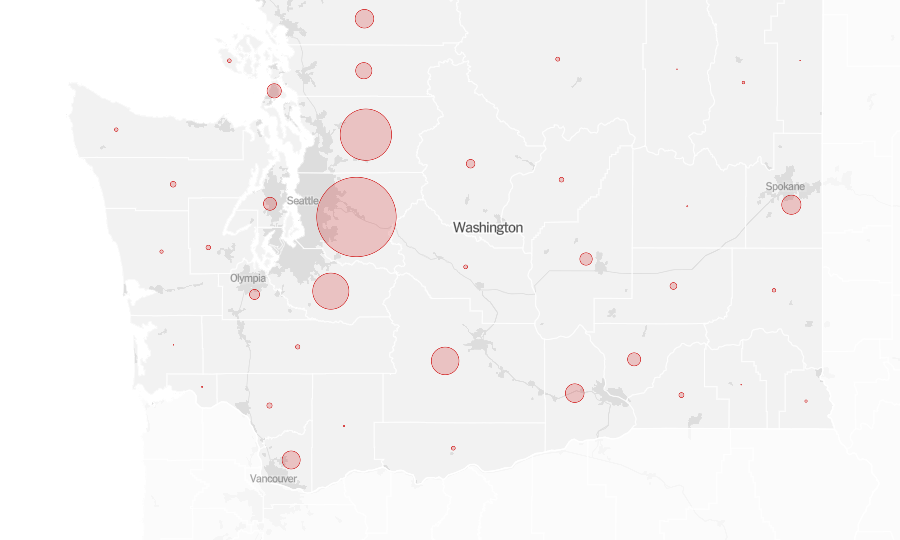
Strong social distancing measures in Washington State have slowed transmission and “flattened the curve” of cases that otherwise would have spiked exponentially, leading to more deaths and overwhelming the care delivery system. The peak of cases is now expected in mid-April in Seattle. The U.S. Army has set up a field hospital there with 250 beds to treat non-COVID-19 patients, and another is being set up on soccer fields to assess and care for sick COVID-19 patients who do not need of ICU-level care, but a safe and supportive place to recover. Nurses from Kaiser Permanente have volunteered to staff the field hospital during an expected surge in cases. King County has rented hotels to house first responders.
The stress on the Seattle health care workforce remains intense, but the commitment to social distancing coupled with the investment in preparation, sharing data, modeling, expanded testing, telehealth and other digital technologies, and creatively acquiring personal protective equipment have helped prepare Seattle for the expected surge while flattening the curve — a relatively good result until a vaccine can be found.